Could you have an irregular heartbeat and not know it?
Contributed to by Dr Ross Walker and published by healthfulforu.com
Have you ever felt your heart beat faster for no clear reason? Maybe it flutters for a few seconds, then settles back to normal. It might happen when you’re resting, watching TV, or walking to the train.
Most of the time, these moments are harmless. But sometimes, they can be a sign of a common heart rhythm condition called atrial fibrillation (AFib), where the heart beats irregularly and sometimes too fast.
AFib isn’t rare, and it doesn’t always cause obvious symptoms. That’s why it often goes unnoticed. Understanding what feels different for you makes it easier to recognise small irregularities in your heartbeat.
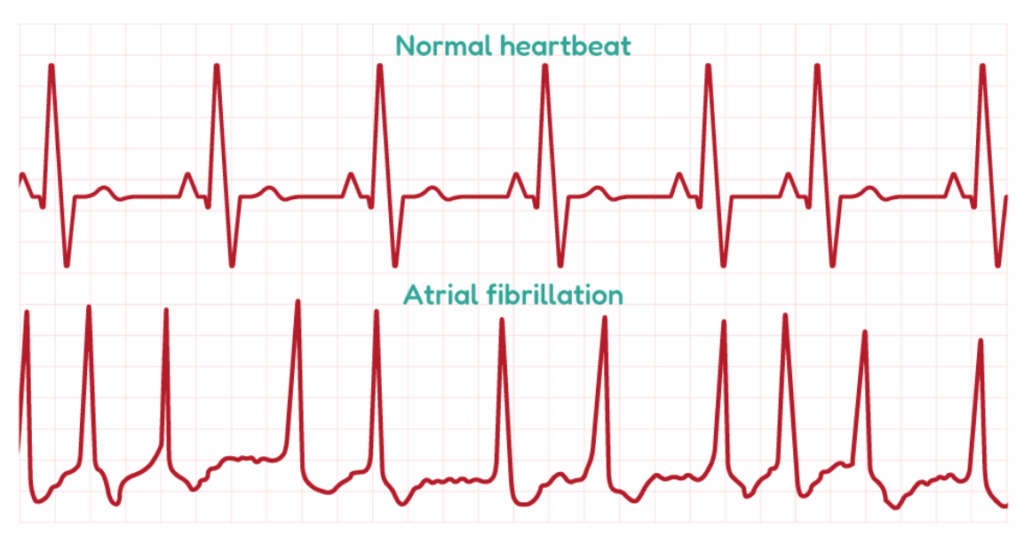
Your heart usually beats in a steady rhythm, regular and coordinated, with the upper and lower chambers working together to pump blood efficiently.
In atrial fibrillation, that coordination is lost. The upper chambers (the atria) start sending rapid, irregular electrical signals, causing the heartbeat to feel uneven, sometimes fast, sometimes skipping a beat.
You might notice this irregular pulse when you’re at rest, reading, or walking up a short flight of stairs. Episodes can last a few seconds or several minutes before settling back to normal. Because these sensations pass quickly, most people don’t think much of them and simply just move on with their day.
EXPERT INSIGHT
Atrial fibrillation (AFib) differs in important ways between younger and older patients, and these differences shape how treatment plans are developed.
According to cardiologist Dr Walker, AFib in younger patients is often linked to lifestyle factors or underlying structural heart abnormalities, and it tends to present in a paroxysmal (intermittent) form. A stronger genetic component is also more common in this group. For those with a history of recurrent AF, ablation is frequently considered as a first-line therapy, as it can be particularly effective in restoring and maintaining normal rhythm.
In older adults, AFib is more likely to be persistent or permanent and is often complicated by other comorbid conditions. For patients over the age of 65 with either paroxysmal or chronic AFib, oral anticoagulation is generally recommended to lower the risk of stroke, unless significant bleeding risks are present. In such cases, left atrial appendage (LAA) closure may be considered as an alternative.
Another important consideration, especially in patients with a high ventricular rate or persistent symptoms despite therapy, is ablation of the atrioventricular (A-V) junction combined with the insertion of a permanent pacemaker. This approach can reduce the symptom burden and lower the risk of progression to heart failure.
Who is more likely to develop AFib?
AFib can affect anyone, but some people are more prone to it because of age, lifestyle, or health conditions that place extra strain on the heart.
Older adults
Age is the biggest risk factor. The likelihood of AFib increases steadily after 50 and becomes increasingly common after 65, as the heart’s electrical system naturally changes with age.
People with hypertension (high blood pressure)
Prolonged pressure on the heart can make the atrial walls to thicken and lose flexibility, which may disrupt normal electrical signalling.
People with other forms of heart disease
AFib often occurs alongside with other heart conditions, such as:
- Coronary artery disease
- Heart valve disorders, especially mitral valve problems
- Heart failure
- Past heart attack or cardiac surgery
People with thyroid or metabolic disorders
An overactive thyroid (hyperthyroidism) can trigger AFib by speeding up the heart’s activity. Diabetes and obesity also raise the risk by promoting inflammation and structural changes in the heart over time.
People with obstructive sleep apnoea
Obstructive sleep apnoea, where breathing repeatedly stops during sleep, causes dips in oxygen levels and extra strain on the heart, which can increase the risk of AFib.
People who drink heavily or frequently
AFib episodes can be triggered by alcohol, sometimes called “holiday heart syndrome.” Binge drinking or regularly exceeding recommended limits, such as more than one drink a day for women or two for men, can increase the risk, especially over time.
Too much or too little exercise
While regular exercise protects heart health, very high levels of endurance training can have the opposite effect. Long-term, intense exercise, such as years of marathon running or triathlon training, may increase AFib risk by stretching the heart’s upper chambers. On the other hand, too little activity can also raise risk indirectly through conditions like obesity or hypertension.
People with a family history of AFib
Having a close family member with AFib slightly increases your own risk, suggesting a possible genetic link.
People with other long-term medical conditions
Chronic lung disease, kidney problems, or inflammatory disorders can increase AFib risk by causing ongoing strain and inflammation in the heart.
AFib is most common among older adults and people with hypertension, diabetes, or heart disease, but it can also occur in younger, otherwise healthy individuals. In these cases, episodes are sometimes triggered by factors such as acute illness, lack of sleep, heavy alcohol use, or periods of high stress.
EXPERT INSIGHT
Atrial fibrillation (AFib) can have a major impact on long-term heart health, raising the risk of complications such as stroke and heart failure. It’s the cause of about one-third of strokes and can also contribute to the development of heart failure. Chronic AFib may lead to structural changes in the heart, including left atrial enlargement, which further worsens the condition.
Steps to reduce risks
- Stroke prevention: The CHA₂DS₂-VASc score, available online, helps assess an individual’s risk. A score of more than 0 for men or more than 1 for women generally indicates the need to begin lifelong anticoagulation therapy. Anticoagulants significantly reduce the risk of stroke.
- Restoring rhythm and improving function: Returning suitable patients to normal sinus rhythm can improve cardiac function and reduce the burden of heart failure. Specific medications are also available that improve heart function, reduce symptoms, and support long-term survival.
- Lifestyle modifications: Regular physical activity, maintaining a healthy weight, following a heart-healthy diet low in sodium and rich in fruits, vegetables, and omega-3 fatty acids, and limiting alcohol intake all lower the risk of complications.
- Regular medical check-ups: Routine follow-ups are important to monitor heart health, manage co-existing conditions, and adjust treatment as needed.